Content
BY DR ZUNAID ALLI / 04 JUL 2019
https://aestheticsjournal.com/feature/case-study-vascular-compromise

Here, we provide a case study of a filler complication and therapeutic strategies.
This article will detail a vascular issue that developed after hyaluronic acid filler was injected into the anterior cheek. Although many practitioners would not encounter an acute presentation of a problem like this, it is crucial to be ready in case one does. As a result, the essay will emphasise the significance of having the emergency kit on hand in order to treat right away, restore blood flow, and so avoid tissue anoxia, ischaemia, and necrosis.
The evaluation and treatment strategy
Following a consultation, a 35-year-old female patient arrived for an injection of dermal filler into the anterior cheek. Three months before, another doctor had treated her medial and lateral cheeks with the proper volumizing hyaluronic acid filler. She was pleased with the procedure’s medial and lateral cheek projection, but she thought the anterior cheek required extra projection because it looked flat from the side. The preceding session did not include any treatment for the anterior cheek region.
According to the patient’s medical history, they were otherwise in good health, did not smoke, and had not had any alcohol in the days before the treatment. Penicillin allergy and prior stomach sensitivity to nonsteroidal anti-inflammatory medications were both established conditions (NSAID). According to the patient’s aesthetic history, she had lip filler, upper face toxin, and minor lumps removed with hyaluronidase.
The region that will be treated was designated and cleaned with a chlorhexidine solution prior to the treatment. The idea was to use the product supplied with 27 gauge needles to inject the volumizing filler (0.3% lidocaine) indicated for the cheek in a direct injection to the periosteum with a small dose of approximately 0.1ml–0.3ml per cheek.
The complications and procedure
First, the right cheek was treated. Without any flashback in the needle hub, the needle was positioned onto the periosteum and aspirated for 10 seconds. Injections totaled 0.2 millilitres. The minor bleeding at the injection site stopped when light pressure was applied. There was no visible bruise.
To ensure the filler was applied in the best possible way, the region was massaged. The patient was pleased to see a decent resulting projection of the right anterior cheek when it was exhibited to her. The left side was made ready for treatment after the syringe’s needle was changed to a fresh 27 gauge needle as supplied. The filler injection process started once the needle was positioned on the periosteum and aspirated again for 10 seconds without a flashback in the needle hub.
When acute skin alterations, colour loss, and blanching were noticed, approximately 0.1ml of filler was injected. The patient had discomfort of a 5/10 at the injection site, and the anterior and lower cheek on the left side went pale. The region involved the upper lip and the region medial to the nasolabial fold. The patient was informed that a problem had occurred, the injection was promptly halted, and the needle and syringe were withdrawn. The most likely cause was determined to be an injection into the infraorbital artery’s vascular area or vasculature. During investigation, capillary refill time was found to be six seconds over the afflicted area, compared to the typical 1-2 second range.
The patient was reassured that the procedure would be abandoned and that emergency care would start right away. The patient grew concerned, but was reassured that the issue could be properly managed. Luckily the emergency kit was to hand, which needed to include hyaluronidase, water for reconstitution, and a heat pack, among other things. The region was wrapped in a warm gauze pack to promote vasodilation while the hyaluronidase was reconstituted.
To ensure appropriate coverage of the afflicted area, the hyaluronidase 1,500 IU was reconstituted with 2.5ml of normal saline to a concentration of 60 IU/0.1ml in accordance with the ACE Group consensus paper4. Using a 30 gauge needle, the hyaluronidase solution was injected at four locations within and surrounding the injection site. The remaining solution was injected in 0.1ml aliquots spaced 5–10mm apart along the vasculature in the region of the mid and lower cheek, as well as the upper lip.
After four minutes of hard massaging, the region started to blanch, at which point a hyperaemic response was noticed. Five to eight minute intervals were used to alternate between applying warm gauze and massaging the region for a total of 75 minutes. It was not necessary to use the second vial of hyaluronidase, which was reconstituted and set aside for future infiltration.
Due to NSAID stomach sensitivity, the patient was apprehensive about taking any aspirin. After receiving hyaluronidase injection, the patient did not report any ocular or periocular pain or visual impairments. The patient additionally reported feeling a little numbness in the nasolabial and upper lip regions, and the patient’s discomfort in the affected location had altered to a burning-type ache.
Overall, the pain level was 6/10, which was considered bearable. With the infiltration of hyaluronidase, capillary refill time improved, going from three seconds at 20 minutes to two seconds at 75 minutes.
After treatment
The patient was examined the next day and given the prescriptions for prednisolone 20 mg every day for four days to treat inflammation and clarithromycin 500 mg twice daily for 14 days as a preventative measure against a probable infection. Co-codamol (30/500), two pills every six hours, or as needed, was used to treat pain.
During examination, the affected area displayed noticeable bruising as well as subconjunctival bleeding on the affected side. Two seconds were needed for capillary filling, and livedo reticularis was seen in the vicinity. A test of visual acuity revealed no ocular or periocular pain and that it was normal. Bilateral neurosensory testing revealed that they were both healthy.
The patient received consolation and a lotion containing vitamin K oxide to be applied topically to lessen bleeding. The swelling surrounding the area was gradually going down when reviewed and evaluated on day three, and the pain level was a 2/10 with some numbness over the cheek. This was most likely brought on by the inflammation of the soft tissues after hyaluronidase injections. The patient was advised to take prednisone for an additional six days.
In comparison to day one, the oedema and bruises were around 50% less on day five, and the subconjunctival haemorrhage had nearly entirely disappeared. The patient’s lip could be felt, and the infraorbital area only had minor bruises.
The inflammation in and surrounding this area in particular was decreasing, and the lower region had a capillary refill time that was typical. Throughout the course of the treatment, the patient was checked on every two to three days, examined, and reassured daily. By day 14, the bruising and swelling had healed and there were no longer any symptoms. The patient is still being closely watched over.
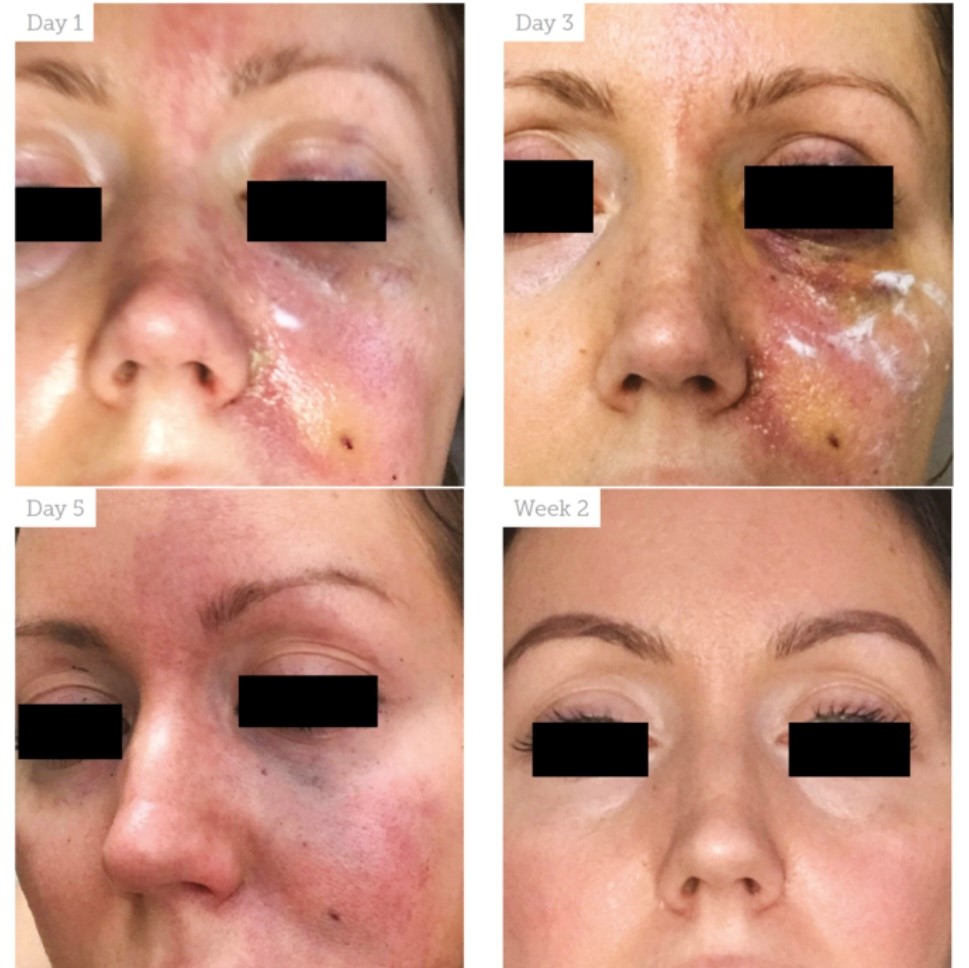
Figure 1 shows the patient’s experience with the problem from the first day to two weeks later.
Discussion
The use of early hyaluronidase in preventing skin necrosis after dermal filler treatment is described in a report of two case studies.5 The study also states that skin necrosis is the most significant complication following dermal filler injection in areas with terminal vascular circulation.5 As a recommendation, aspiration during infiltration is advised. This was done bilaterally before injection, then the right needle was changed after treatment to do a “dry aspirate.”
Despite the failure of both aims, the complication nevertheless happened. Further research has revealed significant variations in the reliability of true positive results following aspiration tests, with one study reporting a reliability of 53%6 and a larger study citing a reliability of 33%7; however, the limitation in both studies is restricted to tests that mimic physiological functions.
The possibility of intravascular placement of the syringe needle is not eliminated by withdrawing the plunger from the syringe when there is no visible blood in the syringe, which presents another challenge with aspiration tests.8 The needle may move as the injector adjusts their hand position to apply pressure to the plunger and begin injection.
Pain and changes in skin colour are the two main diagnostic signs of vascular occlusion, both of which were present in this case. Smaller needles and large bolus injections sent deeper into tissues for volume enhancement increase the risk of vascular events.10
Educating details
Even the most skilled practitioners sometimes face complications, and each time one does, critical considerations are brought to light. The following are the key takeaways from this instance:
Recognise any urgent issues, particularly vascular ones, and take appropriate action. Keep your cool.
Experienced injectors should make sure they follow the most recent guidelines for handling complications, while new injectors should make sure they attend courses where problems are covered in detail. All practitioners need to brush up on their knowledge and stay current with regional best practises and available research.
Give the patient reassurance and let them know that a complication has happened. This includes thorough descriptions of the complication’s primary causes and recommended management strategies in order to provide the best care.
Provide contact details that are easy to reach, even after hours.
A patient with eye problems needs to be referred to an ophthalmologist, therefore make sure the referrals are made as soon as possible.
Throughout the patient’s course of treatment, preserve comprehensive documentation of your communications with them. Because they were thoroughly explained to her during the consultation, the patient in this instance was kind enough to acknowledge that difficulties do occasionally arise. She was still extremely concerned about potential long-term harm or delayed effects, though.
Make sure any steroid, antibiotic, vasodilator, analgesic, and other adjunctive treatments are prescribed and given out right away.
To avoid unnecessary delays, make sure the injector’s emergency kit is accessible and has all of its consumables and up-to-date items.
While injecting filler, try to utilise dermal cannulas whenever possible to reduce risk, especially in risky locations like the glabella, the anterior cheek, and the nasolabial folds.
Do not rely solely on aspiration. A negative aspiration does not rule out the possibility of vascular involvement, as demonstrated by this case.
Summary
It is crucial that the practitioner be familiar with the anatomy of the vasculature, the vascular area, and has a dermal filler emergency kit on available because vascular difficulties may occasionally occur when injecting dermal fillers. To prevent additional effects like necrosis and tissue loss, it is important to quickly identify complications, especially vascular ones, and to promptly treat them.
References
Guidelines of the ACE Group. http://acegroup.online/guidelines ACE Group Emergency kit v2.2
The ACE Group Emergency Kit, Emma Davies and Martin King. <http://acegroup.online/guidelines/
Peripheral Vascular Disease by Steven McGee MD, Evidence-Based Physical Diagnosis, Fourth Edition, 2018.
The use of hyaluronidase in Aesthetic Practice (v2.4) by Martyn King, Cormac Convery, and Emma Davies was published in Journal of Clinical and Aesthetic Dermatology 11(2018), E61-E66.
Early Hyaluronidase use in preventing skin necrosis after treatment with dermal fillers: Report of two cases, Francesco Ciancio, Maria Stella Tarico, Giuseppe Guidice, and Rosario Emanuele Perrotta
Gabriela Casabona, Deramtologic Surgery: Blood aspiration test for cosmetic fillers to avoid unintentional intravascular injection in the face. 2015 July. 41(7): 841-847
Sensitivity of aspiration as a safety test prior to injection of soft tissue fillers, Jani AJ Van Loghem, James J Fouche, and Job Thuis, J Cosmet Dermatol. 2018;17:39-46.
Carey W. and Weinkle S., “Are we safe when the plunger of a hyaluronic acid syringe is retracted before injection?”
2015 December; 41 Suppl 1:S340-6 Dermatol Surg
Aesthetic Plast Surg. 2018 Apr;42(2):498-510. Urdiales-Gálvez F, et al., “Treatment of Soft Tissue Filler Complications: Expert Consensus Guidelines.”
Vascular problems caused by injectable fillers, Part 2: Claudio De Lorenzi, Cosmetic Surgery Journal, vol. 34(4) 584-600