Content
BY DR BEATRIZ MOLINA / 03 JUN 2020
https://aestheticsjournal.com/feature/case-study-necrosis-management
In this article, we’ll look at how to treat skin necrosis on the nose after hyaluronic acid filler injection.
As a cosmetic procedure to temporarily lessen the depth of wrinkles or to contour faces, facial fillers are incredibly popular.
Nonetheless, there is always a slight chance of vascular problems such intra-arterial injection of filler substance, even in the hands of very skilled injectors.
This is a case report of a patient treated who, following an injection of hyaluronic acid filler, displayed symptoms of vascular blockage in the right angular artery and evidence of approaching skin necrosis.
Case study
A 30-year-old woman had her nose reshaped with a 25 gauge cannula and a 20 mg/ml hyaluronic acid (HA) filler with lidocaine. Initially, 0.1ml of lidocaine was superficially administered on the tip of the nose to increase the patient’s comfort at the cannula entry point. Neither during nor immediately following this injection, the patient expressed any complaints of pain or discomfort.

Figure 1: The patient before to therapy
The nasal dorsum was next injected with 0.2 ml of HA, and there were no obvious anomalies. The skin started to blanch as soon as another 0.1ml was applied to the right side of the nose.
The cannula was withdrawn and additional injections immediately ceased. When the patient was questioned about her level of pain or discomfort, she stated that she was not. The patient’s skin was being evaluated for vascular refill at the same time. The time it takes for colour to return to an external capillary bed after pressure is applied to create blanching is known as the capillary refill time. The patient’s capillary refill time was drastically lowered, which was a sign that the vessel was damaged. At this point, there were no other warning indications.
The patient was made aware of the issue and instructed to start hyaluronidase treatment right away. Notwithstanding this advise, the patient insisted on delaying hyaluronidase treatment in order to monitor any potential complications. She consented to wait in the clinic lobby for 30 to 60 minutes before reassessing.
Further skin alterations were seen after 30 minutes. Right angular artery-corresponding livedo reticular patterns were seen on the right side and tip of the nose. The patient claimed that the tip of the nose was sensitive, and the discoloration began to spread to the rest of the nose (Figure 2).

Figure 2: A patient who presented with livedo reticular patterns and discolouration 30 minutes after treatment.
At this point, the patient consented to the use of hyaluronidase to dissolve the HA filler. Initially, a cannula and needle were used to inject 1,500U of hyaluronidase diluted in 1ml of sodium chloride, making sure that the region was thoroughly coated.
There was immediate reperfusion in the remaining locations, and the soreness in the tip had improved. After receiving hyaluronidase treatment, the patient spent 30 minutes under an LED light. The idea behind LED phototherapy is that light may affect and be absorbed by living cells. The procedure’s regenerative and anti-inflammatory qualities have long been acknowledged.
The part that had been hurting before was now pain-free. These measures served as the endpoint for the hyaluronidase treatment since they persisted along with adequate capillary filling. A follow-up appointment was scheduled for the following morning before the patient returned home. The patient returned to the clinic the next day, 16 hours later, and reported feeling better and having no discomfort to report (Figure 3).
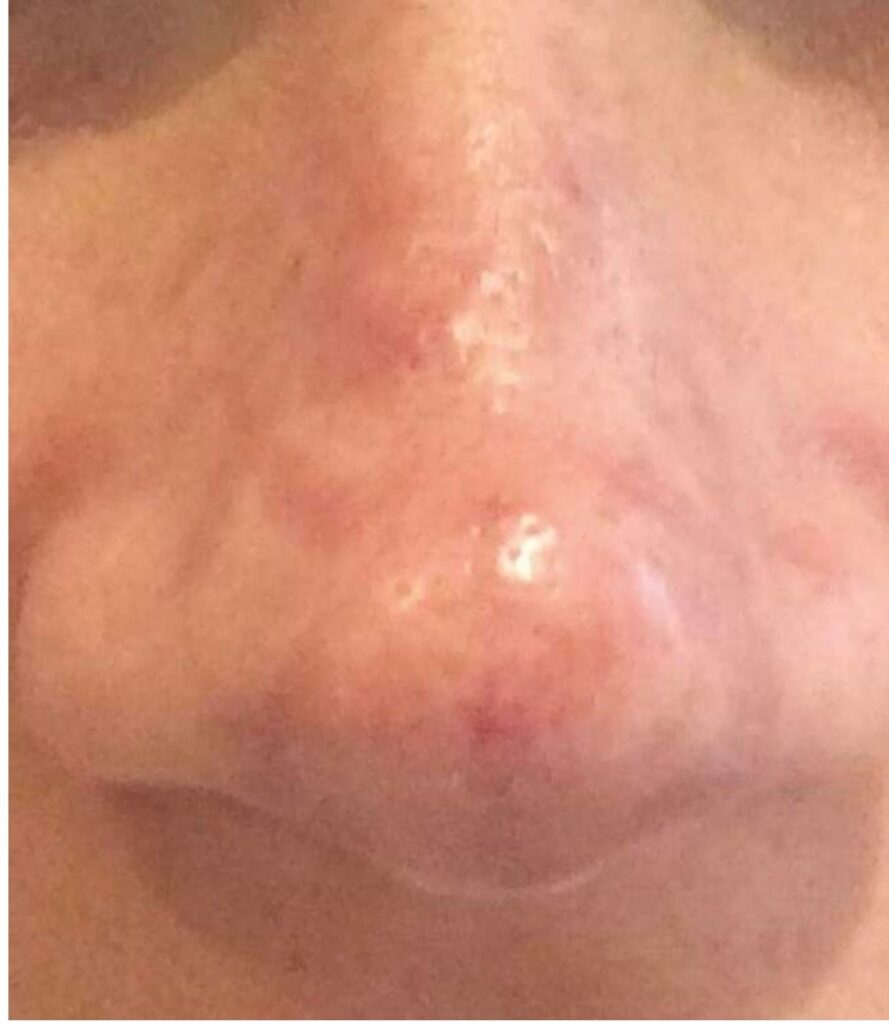
Figure 3: A 16-hour post-hyaluronidase patient
The affected area still had a small discoloration, thus it was decided to continue the hyaluronidase treatment. 750U were superficially injected into the afflicted area of the nose using a 30 gauge needle. Before being released, the patient spent another 30 minutes under the LED.
A second follow-up consultation was scheduled for the following day. 24 hours later, the patient called the clinic and said that everything had calmed down and there was no longer any pain. She was told that she should still return to the clinic for another assessment, but she declined to do so because she preferred to call the clinic with any problems.
She also enquired as to when she may undergo another dermal filler procedure. She was informed that she needed at least six weeks for the area to properly heal before she could have it done, so a follow-up appointment for more treatment was scheduled.
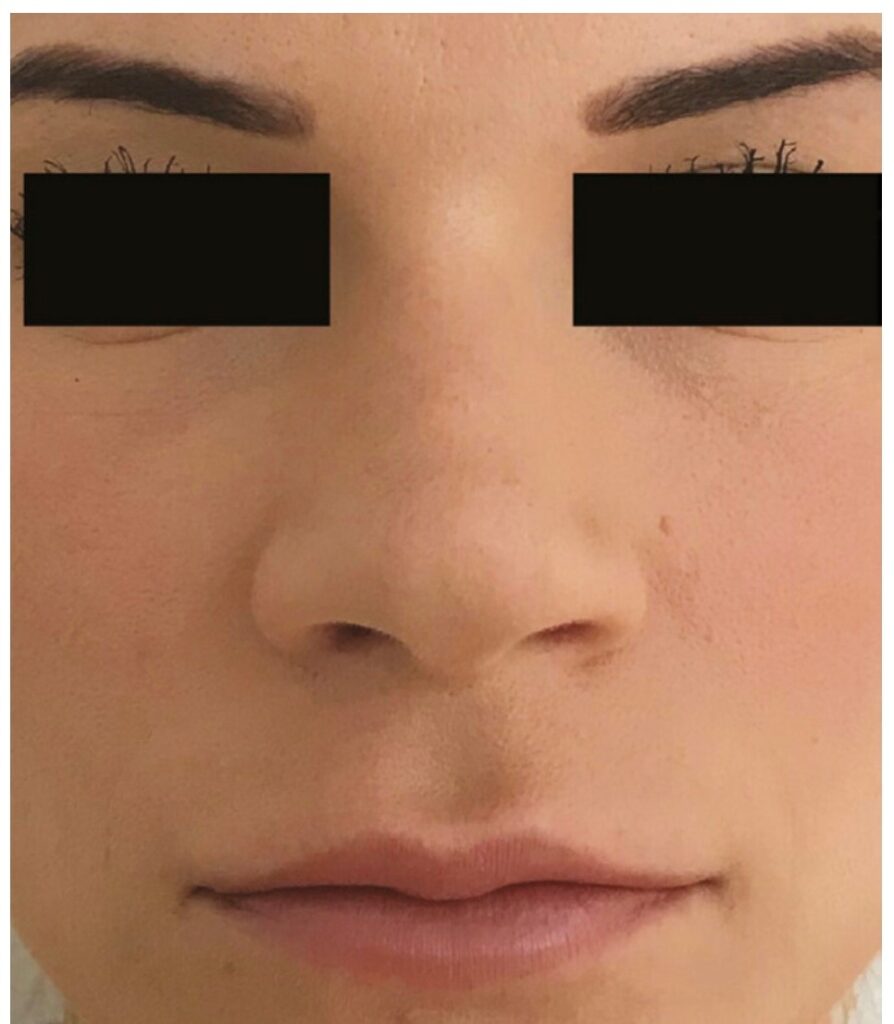
Figure 4: Six weeks after the procedure
Discussion
This patient’s intravascular filler injection case is being shared so that other injectors can learn to see the early symptoms of ischemic skin necrosis and begin treatment right away. Blanching, a livedo pattern, and generally discomfort are signs of intra-arterial injection.2,3
Blanching is typically described as temporary or lasting only a few seconds, 2–5, as it did in this instance. Yet, if the practitioner is not carefully and consistently examining the skin when injecting, they may very frequently miss this. Poor capillary refill perfusion, with or without tenderness, can be used to diagnose vascular episodes early on before more obvious livedo reticularis develops.2-5 Pain is a key indicator of intra-arterial filler injection, but the patient may not recognise it because most modern fillers contain local anaesthetic.
In order to treat the entire area with hyaluronidase, it is helpful to identify the potential arterial territory involved. The nasal skin changed as a result of the angular artery being damaged in this instance (Figure 2).
An essential tool for treating cutaneous issues caused by intravascular HA filler is hyaluronidase. Every aesthetician who performs injectable procedures needs to have this product on hand.6 The estimated dose of hyaluronidase varies depending on the area treated and the type of filler used.7 A minimum of 750U of hyaluronidase must be used for each vascular territory.2-5,8 There is, however, disagreement regarding the recommended dosage and the time between doses in the literature.
In order to prevent skin necrosis and scarring, intra-arterial filler injection should be treated as soon as the diagnosis is made, and no later than 72 hours after the diagnosis.4
The general idea is to inject an adequate amount of hyaluronidase at high concentration levels to dissolve the HA material present in that vascular territory. Expert consensus reports suggest injecting hyaluronidase on an hourly basis until the endpoint of treatment shows reperfusion of skin and correction of blanching/livedo, as well as no pain present in the affected area.
Summary
Even the most skilled injectors occasionally have complications. The fact that the affected area totally recovered from the vascular event suggests that high-dose hyaluronidase might be used to completely reverse the ischemic skin alterations brought on by potential intra-arterial injection or compression. Due to obstruction of the cutaneous vascular supply, which could result in ischemic skin necrosis, intra-arterial injection of filler material has the potential to cause considerable damage.
All injecting practitioners should be able to immediately identify the signs of such complications in order to take appropriate treatment, even though prevention of vascular difficulties by extensive study of vascular architecture is vitally crucial.
References
Phototherapy Using Light Emitting Diodes by Glynis Ablon, J Clin Aesthet Dermatol. 2018 Feb; 11(2): 21–27.
DeLorenzi C. Vascular problems associated with injectable fillers, part 2. J. Aesthet. Surg. 2014;34:584–600.
DeLorenzi C. Novel high dosage pulsed hyaluronidase protocol for vascular adverse events associated with hyaluronic acid fillers. Surgical Arts J. 2017;37:1–12.
Biesman BS, Dayan SH, Cohen JL, et al. Hyaluronidase treatment for imminent necrosis brought on by hyaluronic acid fillers is often advised. J. Aesthet. Surg. 2015;35:844–849.
Impending skin necrosis following dermal filler injection: A “golden period” for first-aid intervention, Hong JY, Seok J, Ahn GR, Jang Y-J, Li K, and Kim BJ. dermatological treatment. 2017;30:e12440.
Patient factors impacting dermal filler complications: prevention, assessment, and treatment. De Boulle K, Heydenrych I. Dermatol Clin Cosmet Invest. 2015;8:205–214.
Durability, behaviour, and tolerability of 5 hyaluronidase products by Casabona, G. MD. Dermatologic Surgery, Volume 44, Issue 11, Pages S42–S50, November 2018.
Global Aesthetics Consensus Group members Signorini M, Liew S, Sundaram H, et al. World aesthetics consensus: evidence- and opinion-based evaluation and consensus recommendations for avoiding and managing problems from hyaluronic acid fillers. 137:961e-971e, Plast Reconstr Surg, 2016