Content
BY ALICE HENSHAW / 12 JUN 2020
https://aestheticsjournal.com/feature/case-study-lip-filler-infection-and-nodules
Here, we go over how we discovered and effectively handled a problem with the lips.
A 45-year-old female patient sought assistance after experiencing an adverse response to dermal filler injections performed on her upper and lower lips by an international clinic for aesthetic purposes. Her history and the reasons behind her lip filler treatment were discussed during the initial consultation. The patient’s initial cosmetic dermal filler injection had taken place. Concerned with excessively inflated lips, the patient looked into clinics and decided on a reputable business in California with board-certified dermatologists. She paid more than was necessary for the procedure in the hope that the best product would be used and that a qualified practitioner would administer it to her.
The patient’s consultation did not offer sufficient post-treatment care and advice or a thorough explanation of the filler type that was used. One hour after the procedure, the patient called the clinic and asked why her lips were uneven and sore. She was told that this was because she had not massaged her lips.
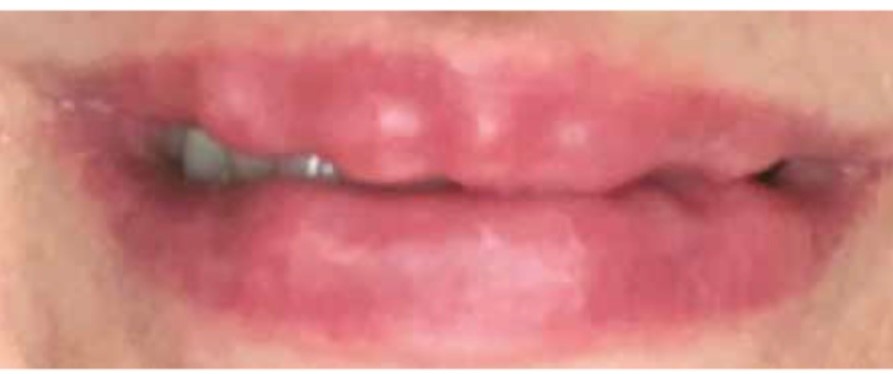
Back in the UK three months after finishing treatment, the patient was having trouble speaking and was afflicted with painful lumps and swelling at night. The patient went to a local beautician, who made incisions in the upper and lower lips in an effort to press the lumps out. Increased pain, infection, and oedema were the only outcomes.
Four months after the procedure, the patient visited a Harley Street clinic, with uncomfortable, swollen lips that interfered with her day-to-day activities, including work and socialising.
She felt she couldn’t leave the house because of embarrassment, so she stayed at home as her anxiety got worse (Figure 1).
Time and unfavourable outcomes
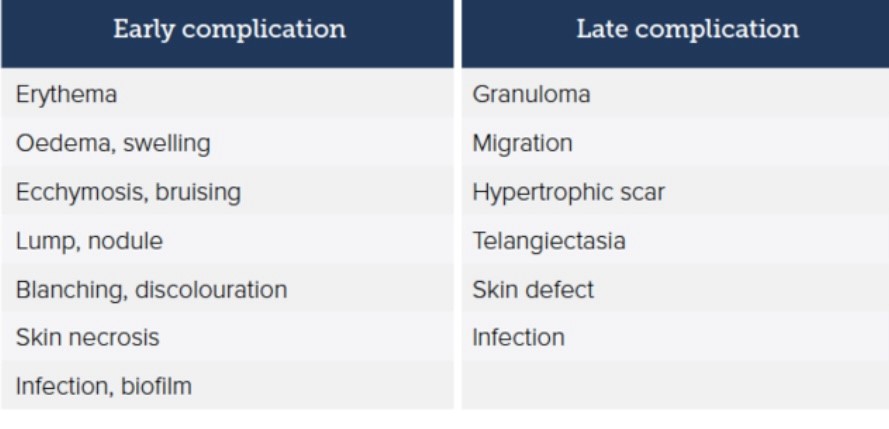
During the consultation, the patient supplied a chronology that helped with the diagnosis because some adverse reactions happen right away after filler injections while others don’t. Figure 2.1 displays the different forms of post-filler therapy problems and their potential onset times.
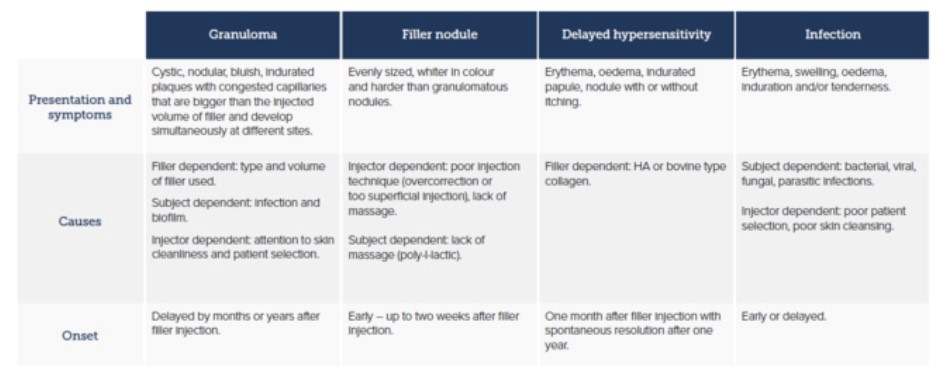
The patient had a serious lip infection, according to the initial assessments. It was possible to feel and see uneven surfaces through the swelling after carefully manipulating the upper and lower lips, which were painful to the touch. It needed to be determined whether the lumps were filler nodules, granulomas, or delayed hypersensitivity because the discomfort and swelling had appeared weeks after the injection. Figure 3.2 gives descriptions of how they present.
Controlling the infection comes first.
Soft-tissue filler injections can induce infection, as can any procedure that penetrates the skin.3 As prolonged inflammation or infection that results in the development of a granuloma can impede wound healing, infection control is crucial.
Erythematous nodules, which are numerous red and tender lumps that last longer than a few days after treatment, may be indicators of inflammation.6-8 There is also a risk for infection with swelling after filler injection and subsequent abscess, but this is outside the purview of this article as it did not happen with this patient. Additionally, wound infections are frequently associated with aesthetically and functionally unfavourable scarring.
A 14-day course of amoxicillin/clavulanic acid was recommended as the initial course of treatment. Before a well-informed choice could be made about how to treat the lumps, the pain and swelling had to be reduced, regardless of whether the infection was a secondary cause of the filler nodules or the primary reason for potential granulomas.
Antibiotics were prescribed in addition to lump treatment because it was possible that the lumps were filler nodules. The use of hyaluronic acid (HA) based filler was confirmed by the original clinic, allowing for hyaluronidase treatment. Hyaluronidase should be administered cautiously if infection is also suspected since it may cause the infection to move further along the tissue plane9. This, along with the patient’s safety, was the motivation behind attempting to treat the infection before treating the wound. The infection had been cured, the patient’s lips had shrunk to a normal size, and the suspected filler nodules were much more noticeable when the patient showed up for her second appointment two weeks later (Figure 4).
Step two is to locate the lumps.
The swelling and some of the discomfort had subsided over the two-week follow-up, but the lumps persisted. Hence, before starting treatment, it had to be determine what was causing the lumps. Granuloma, delayed sensitivity, and filler nodules were among the potential explanations that were examined.
Granuloma
Granulomas, a chronic inflammatory reaction with various aetiologies, can be defined as a tumour made up of a collection of immune cells, primarily macrophages. Granulomas are relatively uncommon complications, with a frequency of occurrence reported as 0.02-0.4% after HA use for dermal filler in the dermis.
Macrophages are activated and fused into multinucleated giant cells12,13 in the case of foreign body granulomas, which happen six to 24 months after filler injections.14-16 Given that the lumps were early complications for this patient and that cystic granulomas are relatively uncommon, the diagnosis of cystic granuloma was ruled out.
Slow sensitivity
Very few injection-related side effects persisted after hyaluronic acid replaced bovine collagen in dermal filler procedures, however non-allergic local side effects like discomfort, bruising, and temporary oedema are common. It has been proposed that the anticoagulant effect of HA, which shares structural similarities with heparin, is the reason why HA fillers produce more swelling and bruising than collagen fillers.18 They typically go away in a few days and normally don’t require treatment.19,20
Skin erythema that develops right away after an injection is typically temporary and normal. Nevertheless, erythema should be distinguished from infection. If erythema persists for more than a few days, it is likely a hypersensitivity reaction. While the patient had no prior history of using dermal fillers, delayed hypersensitivity was taken into consideration; nevertheless, given that the nodules were uniform in size and white in colour, it was more likely that they were filler nodules.
Auxiliary nodules
Immediately following treatment, lumps or nodules commonly take the form of well-contained palpable lesions that are cystic, oedematous, or sclerosing in nature. These lesions can be brought on by over-injecting, injecting too much material, clumping the filler, or dislocating the implant by moving the muscles.21–24
Lips have thin mucosa and are a highly mobile part. Firm massaging and meticulously placing filler in the deep supraperiosteal plane are two precautions taken to prevent visibility of the implanted material.25,26
Visible, pale nodules in the skin may develop if HA filler is injected too superficially or if the product is distributed unevenly.27 This was seen in the patient. The woman was instructed to massage the lumps in her lips after treatment by the original clinic, a clear indicator that the lumps were caused by an improper dermal filler injection technique. Patients should be advised against massaging the area that has received a filler injection due to the danger of infection. After injecting the filler, the practitioner should manually massage the region since they are aware of the proper pressure and technique. It was plausible to consider treatment as HA-based filler nodules because the uneven lumps had appeared right away after treatment and their visual appearance and the likelihood of a HA-related granuloma being present was so remote.
Third step: taking action
10ml of bacteriostatic saline were used to reconstitute 1500 units of hyaluronidase. Ten units of solution were used for a patch test on the patient’s arm, and there were no negative effects. Using a 25 gauge insulin syringe and 10 unit bolus injections, 2 cc of the dilution was then administered into the nodules while massaging the lips. The patient’s lips had greater movement an hour later, and the nodules had shrunk in size. She was instructed to come back in two weeks for a follow-up.
The erroneous filler placement and related infection were successfully treated, according to the two-week follow-up consultation. The patient’s lips showed no signs of irritation or discomfort. To touch, her lips were even and gentle. Undoing the filler placement gave the patient the intended effect, and as a result, she felt confident and healthy (Figure 5).

Summary
This research has focused on the differential diagnosis of nodules resulting from injections of dermal fillers. Despite the fact that this patient did not have delayed hypersensitivity or dermal filler granulomas, it is crucial that the aesthetic injector is meticulous in minimising the circumstances that could lead to their development.
Prompt cleansing and disinfection of the skin, sterile injection technique (avoiding injection through any nasal or oral mucosa), prophylactic antibiotics, and the use of smaller gauge needles to minimise trauma and access for bacteria are all ways to prevent dermal filler-related granulomas.28 Patients should be advised to refrain from wearing makeup immediately before and after injection.
Avoid overcorrecting with dermal filler, injecting an excessive volume of the incorrect filler for the tissue type, and failing to massage the area enough to redistribute the filler evenly. It is advised to use proper injection technique, set the needle at the right depth before injecting, and stop injecting before the needle retracts.
Every treatment involving the injection of dermal fillers should include counselling the patient and taking precautions including selecting the right filler and preventing infection. Throughout the entire consultation process, the three main components should be patient permission, education, and proper follow-up assistance.
References
Pavicic. & D. Funt (2013). An review of therapy options for adverse occurrences using dermal fillers in aesthetics. Clinical, Cosmetic and Investigative Dermatology, (6), 295–316. <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865975/>.
Cybulska. “Granuloma Management” (2016). Journal of Aesthetics, 3(4), pp. 32–25.
Kim, YJ, and Lee, JM. The pathogenesis, clinical manifestation, histologic findings, and therapy of Foreign Body Granulomas after the use of Dermal Fillers (2015). Pages 232-239 of Archives of Plastic Surgery, 42.
Jin, YW, Kang, BS, and Na, YC. An in vivo study comparing the effects of cellulose and gelatin on wound healing was published in 2012. 39, 317-321, Archives of Plastic Surgery.
Jordan SW, Hanwright PJ, Bilimoria KY, Mioton LM, Kim JY. A multi-institutional analysis of 15,289 patients’ preoperative wound categorization and postoperative infection was published in 2013. Pages 522-429 of Archives of Plastic Surgery, 40.
De Boulle. Treatment of Problems Following Filler Implantation, 2004. pages. 15 in Journal of Cosmetic Dermatology, 3:2.
Lemperle and DM Duffy. Therapy Options for Dermal Filler Problems, 2006. Journal of Aesthetic Surgery, 26, 356-364.
Fagien, S.; Sclafani, A. “Treatment of Injectable Soft Tissue Filler Problems” was published in 2009. dermatology operations. 35, pp.1672–1680.
DeLOrenzi. “Complications of Injectable Fillers” (2013). Journal of Cosmetic Surgery, 1(35), p. 575
Kim, YJ., and Lee, JM. Foreign body granulomas following dermal fillers: pathogenesis, clinical characteristics, and therapy, (2015). the Plastic Surgery Archives. 42, pp. 232–239.
DL Boros and JL Truden. “Collagenase, elastase, and nonspecific protease synthesis by active or immunomodulated hepatic granulomas and granuloma macrophages/eosinophils of mansoni-infected mice,” (1985). <https://www.ncbi.nlm.nih.gov/pubmed/2996360
KM Murphy, P Travers, and M Walport. ‘Janeway’s immunobiology’ (2008). : Garland Science, New York.
JL Farber and E. Rubin. “Pathology and Review of Pathology” (1999). Lippincott-Raven, Philadelphia.
Foreign body granulomas after all injectable dermal fillers: part 1. Gauthier-Hazan, N., Lemperle, G., Wolters, et al. Potential causes’. Surgery for plastic reconstruction. 123, pp.1842–1863.
GT Williams and WJ Williams. GRANULOMATIC INFLAMMATION: A REVIEW (1983). Clinical Pathology Journal. 36, pp.723–733.
Gauthier-Hazan and G. Lemperle. Injectable dermal fillers after all, foreign body granulomas: part 2. Options for treatment. Surgery for plastic reconstruction. 123 pp.1864–1873.
It was written by L. Cerroni, L. Christensen, H. Kutzner, L. Requena, C. Requena, and U. Zimmermann. Adverse effects of injectable soft tissue fillers, 2011. American Academy of Dermatology journal. 1, pp.34.
SV Pollack. Hylaform, Restylane, and Artecoll are three novel injectable dermal filler materials described in 1999. Cutaneous Medical and Surgical Magazine. 4, pp.527-32.
Magnani, A., Lamponi, S., and Renier are the authors. The impact of molecular weight on the biological activity of sulphated heparin-like hyaluronic acids was first reported in 1998. Biomaterials. 19, pp.801-6.
- Hedner and M. Pandolfi. Sodium hyaluronate and sodium chondroitin sulphate’s effects on the coagulation system in vitro were studied in 1994. 864-6 in Ophthalmology, vol. 91.
Ahn, D., Suh, I., Jeong, H., and Kim, J. 2014 publication of “Treatment Algorithm of Complications after Filler Injection: Based on Wound Healing Process.” Korean Medical Science Journal. 29:3. ppS176–S182.
AC Bhatia and JL Cohen. The usefulness of topical vitamin K oxide gel in the healing of postoperative purpura was discussed in 2009. Medications and Dermatology Journal. 8, pp.1020–1024.
Preventing and managing dermal filler problems is the subject of a 2006 article by Gauthier-Hazan, Lemperle, and Rullan. Surgery for plastic reconstruction. 118, pp.92s–107s.
DM Duffy and G Lemperle. Therapy solutions for dermal filler problems were published in 2006. Journal of Aesthetic Surgery. 26, pp.356–364.
- Fagien and AP Sclafani. Management of problems with injectable soft tissue fillers, 2009. Skin cancer surgery. 35, pp.1672–1680.
M Alam and JS Dover. Treatment of problems and sequelae with transient injectable fillers, 2017. Surgery for plastic reconstruction. 120, pp.98s–105s.
An update review of current skin fillers: Cheng LY, Sun XM, Tang MY, Jin R, Cui WG, and Zhang YG. 2016;3:92-99 Plast Aesthet Res. http://dx.doi.org/10.20517/2347-9264.2015.124
Cybulska. “Granuloma Management” (2016). 32–25 in Aesthetics, 3(4).
Special Feature: Make-up After Procedure, S. Kilgariff, Aesthetics (2019), available at this link: https://aestheticsjournal.com/feature/makeup-post-procedure