Content
BY KAY GREVESON / 06 JUL 2018
https://aestheticsjournal.com/feature/case-study-dissolving-filler
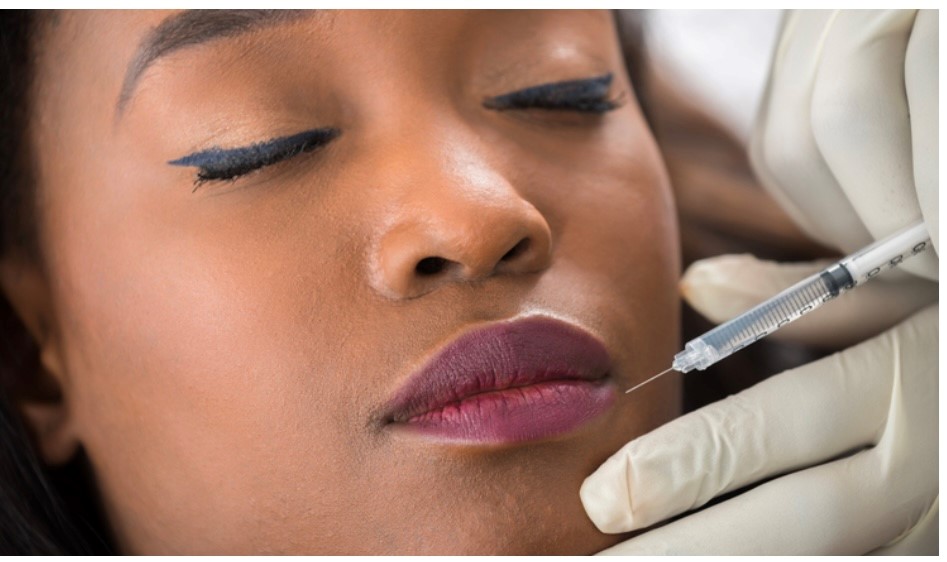
Here, a patient’s overly-treated lips receive lip filler dissolving.
Dermal filler issues, especially those caused by persons who use them without medical training, have received a lot of public attention recently. While undergoing lip augmentation procedures, it’s crucial to take lip anatomy, patient expectations1, and product preference2 into account. You should also avoid overfilling areas. The ratio of the upper to lower lip should be 40:60, with the exception of Afro-Caribbean ethnic group, where the ratio should be 50:50.3 As practitioners we should use no more than 1ml in the first clinic visit in order to prevent over-filling.
Research case
A 28-year-old male patient who is a makeup artist and blogger for YouTube and Instagram visited seeking a more natural appearance for his lips after having them altered elsewhere. He had no known allergies, no known past medical conditions, and wasn’t using any long-term medications. His aesthetic past included receiving unknown doses of hyaluronic acid-based (HA) dermal filler for the lips over the course of a year at another facility abroad. He had no known side effects from the procedure, but even though he initially wanted to give his lips a larger appearance, he now thought they had an excessive amount of volume.

Figures 1 and 2 show images taken before and after therapy, respectively.
The patient knew the dermal filler was HA-based but was unable to recall which specific variety was utilised. Upon assessment, the upper lip was noticeably bigger (Figure 1) and had a ratio of almost 60:40, which is the opposite of that advised. Dermal filler had penetrated to the cutaneous upper lip and was felt in the lip. The dermal filler that had been utilised, was seemingly, “too thick” for the area injected, and the lip felt extremely stiff to the touch.
It seemed reasonable to employ hyaluronidase to remove the extra filler because the upper lip was sticking out. There were concerns the patient might have some body dysmorphia. This was discussed with him and inquired as to why he had so many procedures done on his lips. He confessed that he receives many complimentary treatments as part of his profession as a blogger and social media influencer and that it might be challenging to say no.
After discussing the uses, advantages, and hazards of hyaluronidase, photos were taken with the subject’s written agreement. Focus was placed on his expectations for the procedure, the effects of hyaluronidase, and the possibility that it would dissolve his own natural hyaluronic acid rather than just the filler. The ACE group’s standard protocol4 was carried out.
Hyaluronidase 15000iu ampoule was diluted to 300 iu/ml with 5ml of 0.9% sodium chloride. A 0.02ml/6iu intradermal patch test was carried out in the forearm, and when the results were negative after 30 minutes, the treatment was deemed safe to continue. Due to the superficial region, the treatment area was chalked out (Figure 2), and hyaluronidase was injected into the upper lip under the skin using a 30g insulin syringe. Following treatment, the patient was observed for 30 minutes before a follow-up appointment was scheduled for two days later.
48 hours later, the patient was seen again in the clinic when the lips were checked and pictures were taken. Following therapy with hyaluronidase, the patient stated that the dermal filler appeared to dissolve satisfactorily within 12 hours and that the upper lip had restored to its usual size and proportion to the bottom lip. I suggested that he wait two weeks before getting another dermal filler procedure so that the lip could heal and the body could make sure the hyaluronidase had been eliminated.
Regrettably, it was evident via social media a week later that the patient had gone to a different clinic, which was primarily run by non-medical aestheticians, for additional lip enhancement procedures. When contacting the patient and questioning him about going against advice, he said he “did not feel like himself anymore” and had come to realise that he actually wanted larger lips. This could confirm the first body dysmorphia suspicions. In hindsight, it was the right choice to dissolve the dermal filler because they did appear out of proportion to his face. Following this encounter, it’s felt that using a modified body dysmorphia scale in consultations could be helpful.
Conclusion
In this instance, the lips were overcorrected with hyaluronic acid filler, presumably as a result of a bad dermal filler choice, albeit this cannot be proved. Patients’ expectations and reasons for seeking treatment should be taken into consideration by practitioners. To achieve the best results, people must also practice within their areas of expertise and work with tools that they are accustomed to. Social media might affect a patient’s decision to receive therapy and can project erroneous notions of what is “normal.” This may have been the driving force behind this patient’s decision to receive treatment in the first place because of his substantial social media fan base as a makeup artist. It is the duty of practitioners to determine whether a patient is a good candidate for treatment and to provide them with appropriate guidance. In some circumstances, it may be necessary to refuse treatment.
REFERENCES
- S. Robson (2016). Handling the expectations resulting from cosmetic procedures. ACE group direction. Online as of 14/1/18
- Systematic review of “filling” procedures for lip augmentation with regard to material types, results, and complications by San Miguel Morgas et al. (2015). 2015 July;43(6):883-906 J Craniomaxillofac Surgery
- Journal of Aesthetics, Walker L. Online resource accessed at https://aestheticsjournal.com/feature/lip-augmentation
- The Usage of Hyaluronidase in Aesthetic Practice by M. King; 2017 ACE group recommendations. Online as of 14/1/18
- A cosmetic procedure screening questionnaire (COPS) for body dysmorphic disorder was developed by David Veale, Nell Ellison, Tom Werner, Rupa Dodhia, Marc Serfaty, and Alex Clarke in 2012. 65 (4), 530-532 in Journal of Plastic Reconstructive and Aesthetic Surgery. www.dx.doi.org/10.1016